USC researchers study schizophrenia
Researchers from the USC Dornsife College of Letters, Arts and Sciences issued findings Feb. 10 about the function of synapse-associated protein 97, its mutations and relation to schizophrenia formation in the brain.
Schizophrenia is a neurodevelopmental disease which affects 20 million people worldwide and requires life-long treatment and medication. While scientists attribute the formation of schizophrenia to a combination of genetics and environmental factors, the exact cause and location of schizophrenia in the brain is largely unknown.
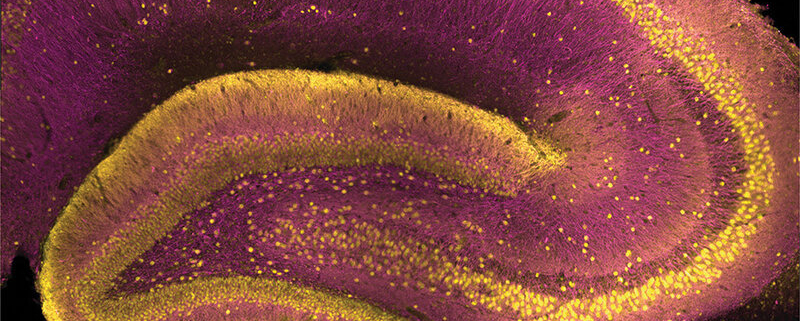
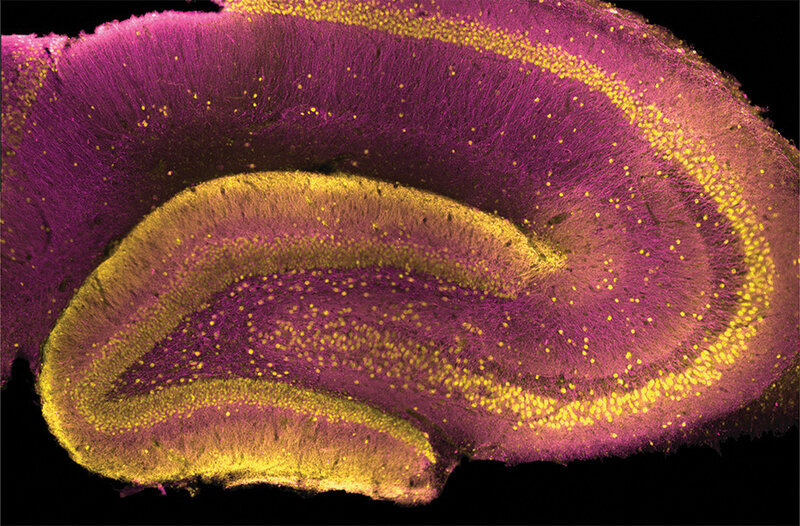
Yuni Kay, a doctoral student studying neuroscience and co-author of the study, said the study is distinct among other research because the findings highlight the importance of analyzing SAP97 in different brain regions. Through research in the dentate gyrus of the hippocampus, the center for memory in the brain, researchers found the molecular and cellular functions of SAP97, which Kay attributed to the lack of variety in the brain regions that were studied in the past.
“Not only do we find the role for this protein, we found out why people weren’t able to figure it out before,” Kay said. “Why didn’t people know what [SAP97] did? Because they were looking in the wrong place. Where is it? It’s in the place where schizophrenia is strongly also implicated. It was like the puzzles were starting to fit together.”
Lea Decarie-Spain, a postdoctoral researcher in the department of biological sciences and co-author of the study, said the physiology work done by Kay and Bruce Herring, an assistant professor of biological sciences and co-author of the study, focused on targeting specific protein codes and genetic expression to replicate genetic phenotypes in rats.
“[The study] is showing what the impact of this protein has on neuronal activity … it’s definitely advancing knowledge just in relation to general neuroscience,” Decarie-Spain said. “I’m hoping that this will bring some new insight into therapies for schizophrenia, because they’ve shown that the specific molecule that they target is highly involved in the risk for schizophrenia.”
When patients with schizophrenia are being treated, they are usually only treated for their symptoms which will “rarely, if ever, cure the disease,” said Anna Pushkin, a doctoral student studying neuroscience and co-author of the study.
Schizophrenia’s symptoms include hallucinations, delusions, flat affect, the loss of a sense of personal identity, poor executive function and deficits in memory. She also said that analyzing contextual memory in the hippocampus would give clues to understanding more about the disorder’s origins.
Pushkin said future steps to curing schizophrenia could include assessing specific mutations of the protein for each symptom and behavioral phenotypes to assist translational research, which healthcare workers can then use to benefit patients. The linkage between mutations and impaired contextual memory is historically linked to the onset of schizophrenia which scientists are able to confirm and investigate more in depth as technology improves.
“There are specific regions that might be more implicated with mutations in schizophrenia,” Pushkin said. “We don’t know the specific mechanisms of what’s going on, where in the brain, what’s happening, where specifically it’s happening, and just knowing fundamentally what’s happening at a synaptic, at a molecular level will help to create treatments for those with developmental disorders.”